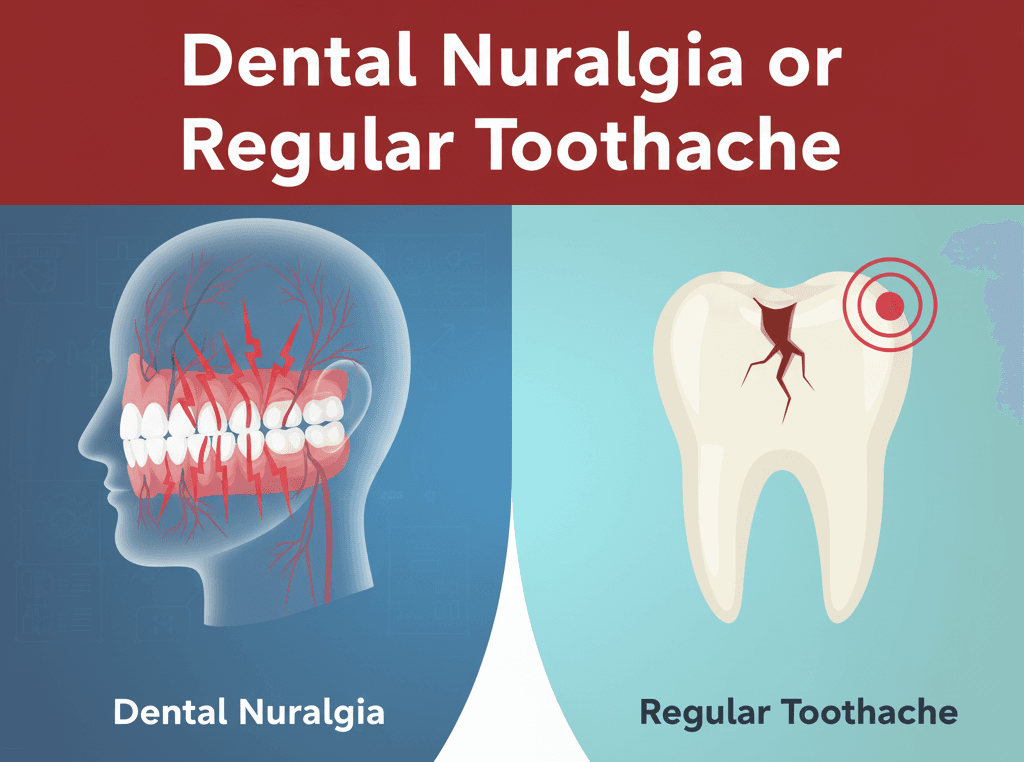
If you have ever been stopped cold by a sudden, searing jolt of pain in your mouth or jaw that feels less like a steady toothache and more like an electric shock, you know how confusing dental discomfort can be. Many people assume it’s just a regular toothache, but sometimes the pain is much deeper — literally. When standard dental pain turns into an unpredictable, debilitating nerve “attack,” it’s time to consider a specific type of discomfort known as Dental Neuralgia. This condition often mimics common tooth problems, but its cause lies in the nerves rather than the teeth themselves. Understanding the difference is key to finding the right treatment and lasting relief.
Table of Contents
ToggleWhat Is Dental Neuralgia?
Dental neuralgia refers to nerve-related pain that affects the teeth, gums, or jaw. Unlike typical toothaches caused by cavities, infections, or gum disease, this condition stems from irritation or damage to the nerves responsible for facial sensation — most commonly the trigeminal nerve. When this nerve becomes inflamed or compressed, it can send sudden bursts of sharp, stabbing pain that feel like electric shocks.
Dental neuralgia can affect one or several areas of the face, including the teeth, gums, cheek, or even the jawline. Because the pain often feels like it’s coming from a specific tooth, it’s frequently mistaken for a dental issue, leading many people to undergo unnecessary treatments before the true cause is identified. This research has documented that among trigeminal neuralgia patients seeking dental treatment, the majority undergo invasive procedures such as extractions that fail to relieve their symptoms, highlighting the critical importance of accurate diagnosis.
Common Causes and Triggers
Dental neuralgia can develop for a variety of reasons, most of which involve nerve irritation, inflammation, or compression. The most common underlying cause is trigeminal neuralgia, a chronic condition where the trigeminal nerve — the major nerve responsible for facial sensation — becomes overly sensitive or pinched. This can happen due to blood vessel pressure, past facial injuries, or even certain medical conditions that affect nerve function.
Other contributing factors can include tooth extractions, jaw trauma, sinus infections, or dental procedures that inadvertently affect nearby nerves. In some cases, nerve pain develops after a root canal, implant placement, or even after prolonged teeth grinding (bruxism), which puts pressure on facial nerves and surrounding tissues.
There are also specific triggers that can set off sudden bursts of pain, such as brushing your teeth, chewing, speaking, touching your face, or exposure to cold air. Even light movements — like smiling or washing your face — can trigger sharp, unexpected jolts of pain. Identifying these triggers is an important step in both diagnosis and management, as it helps your dentist or doctor tailor a treatment plan that minimizes nerve irritation.
Symptoms of Dental Neuralgia
Dental neuralgia can easily be mistaken for an ordinary toothache, but the pain behaves very differently. Below are the most common signs and sensations to help you recognize it:
- Sudden and sharp pain that feels like an electric shock running through the teeth, gums, or one side of the face.
- Burning or shooting sensations that appear suddenly and last only a few seconds at a time.
- Pain triggered by simple actions such as brushing your teeth, chewing food, talking, or even light facial touch.
- Discomfort from temperature changes, especially when drinking cold or hot beverages.
- Episodes of pain that start and stop without warning, sometimes repeating multiple times in a day or even within an hour.
- Lingering soreness or sensitivity after a painful episode, even when the main pain subsides.
- Resistance to typical dental treatments, such as fillings, antibiotics, or desensitizing toothpaste, which do not relieve the pain.
- Additional sensations such as tingling, numbness, or burning around the mouth, jaw, or cheek.
- Difficulty eating, speaking, or resting, especially when pain attacks occur frequently or unpredictably.
- No visible signs of dental problems, such as cavities or gum inflammation, despite severe discomfort.
Conclusion
Understanding dental neuralgia can be life-changing for anyone who has been struggling with unexplained, shock-like pain that doesn’t respond to regular dental treatments. What often feels like a simple toothache can actually stem from nerve irritation deep within the face or jaw. Without proper diagnosis, many people endure unnecessary procedures or prolonged discomfort. Recognizing these specific symptoms—the sharp, shooting quality, the immediate onset and cessation, and the sensitivity to light touch or cold—is the most valuable information you can have in seeking relief.
Understanding that the source of your pain is neurological, not always dental decay, is the necessary first step toward finding an effective solution. You don’t have to manage this unpredictable pain alone. Our dedicated dental team specializes in diagnostic methods that can accurately identify the cause of your nerve discomfort, leading you to the proper nerve-stabilizing treatments or targeted interventions you need. If you are tired of the daily guessing game and ready to find a definitive path to pain relief, we encourage you to schedule a consultation with our dental team today. Let us help you put the sharp, shocking pain behind you and regain comfort and quality of life.